(Pictured: Chelsea Ciano, founder of Family Fit Exercise Physiology, sharing exercise with her daughter!)
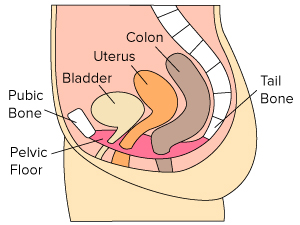
Bouncing on a trampoline or simply laughing at a joke can be a tricky experience for new mums and their pelvic floor muscles. Childbirth places tremendous strain on the body, even if the labour and delivery were relatively straightforward.
Regular exercise offers a range of health benefits for the new mother, including faster recovery from the birth process, faster reestablishment of the abdominal and pelvic floor muscles, increased energy to cope with the demands of a newborn baby, increased ability to deal with stress and depression and, of course, faster return to pre-pregnancy shape and fitness.
Nevertheless, don’t feel any pressure to exercise before you are ready – listen to your body.
It’s important to be well informed before starting postnatal exercise. The focus for a new mother should be primarily on recovery and rehabilitation. This is achieved through strength development, postural alignment, functional stability, core strength, balancing opposing muscle groups and flexibility. Exercise post pregnancy should also be about the well-being of the mother and rewarding the body with the energy it requires to be a great mum.
All too often the focus for new mothers is about ‘losing baby weight’ and ‘getting your body back’, and while these goals are achievable, it’s important to understand that if recovery exercises are rushed or bypassed, future injuries are likely. For example, new mums performing crunches, planks or full push-ups before the abdominal muscles have repaired themselves will cause further abdominal separation and damage.
So my message for new mums is: think rehabilitation. Weight loss and aerobic fitness can wait. And remember that weight loss is largely tackled from a dietary perspective.
Post baby exercise
It is very important to exercise safely and correctly after the baby is born. Your body has undergone nine months of physical and physiological changes and these do not reverse overnight. Many ‘how to get your body back’ programs ignore the maternal adaptations of pregnancy (which can continue for up to six months post-birth) by prescribing exercises that can aggravate and exasperate postpartum symptoms and discomforts, potentially leaving new mothers with unnecessary injury, dysfunction and pain.
It’s best to omit or modify exercises that require fast movements, jumps, lateral movements, fast changes of direction and extremes of joint flexion and extension (e.g. deep squats). New mothers should avoid exercises that cause a bearing down on their pelvic floor, certain abdominal exercises and high impact exercises until core control, pelvic floor strength, bladder and bowel control has been regained. It is best to listen to your own body and if you are unsure seek advice from an accredited exercise physiologist.
Many new mums love the idea of ‘exercising with baby’, however you must be very careful when using your baby as a weight. Often technique is compromised, thus reducing the benefit of the exercise and increasing the risk to mum and baby. I personally love to workout with my baby girl and she enjoys it too. We often use a mirror to observe technique and avoid unstable objects like fitballs, discs and BOSUs.
Mothers constantly push their bodies to their limits – whether it is carrying your baby throughout pregnancy, feeding your baby with heavy breasts or lugging your toddler until they are too heavy to lift. They often put up with upper and lower back pain, unaware of the safe, effective exercises available to minimise their discomfort.
I’m a mum of two and I have experienced firsthand the benefits of a well-organised postpartum exercise program. My second pregnancy was more physically demanding than my first, probably because I had a toddler to look after and I used more of my ‘me’ time to rest rather than exercise. The progression of the pregnancy triggered several debilitating physical conditions and after giving birth I felt weak, soft and tired. A month postpartum I realised I needed to rehabilitate myself if I were to be dynamic mum. Slowly and gradually my post-baby discomforts were alleviated and corrected through prescribed exercise. Eight months on and I am fit, energetic and strong helping me to be a vibrant, active mum.
Specific exercises are required to heal stabilising muscles, correct any post-pregnancy abdominal separation and strengthen pelvic floor muscles. Concentrate on repairing the body first, which can take weeks or months depending on the individual, and then you will be able to fully enjoy being active with your family, and living your best life without any aches, pains or weaknesses.
Always consult with your doctor or midwife prior to commencing any postnatal exercise regime. Whether you are ready or not is dependent on many individual factors. It is recommended that your return to exercise be gradual and that you progress slowly.
My postnatal approach is to primarily:
- Activate your core and pelvic floor muscles.
- Heal abdominal separation (diastasis recti).
- Correct posture.
- Strengthen core and butt muscles.
Vigorous cardio exercise should be avoided until the above has been achieved. Cardiovascular exercise has many benefits, but being exhausted and sore has none, so mum has to be well rested and getting regular restorative sleep.
My recommended modes of exercise are personalised exercise prescription, walking, pram exercises, swimming, Pilates, yoga, cycling and light controlled gym work (preferably with a well-organised program).
New mothers can resume exercise without negatively affecting breastfeeding, provided the mum consumes enough calories to support both breastfeeding and exercise.
An appropriate and supportive bra is essential to any new mum looking to enjoy her exercise. It is best to exercise after breastfeeding, rather than before when the breasts are heavy and full. Don’t perform any exercises that hurt the breasts.
Be careful not to overexert yourself because a tired, sore mum is no fun for anyone. Stop exercise and see your doctor if there are any changes in your lochia.
Don’t expect too much too soon. Many women experience difficulties in losing weight and gaining fitness in the post-partum period. Allow yourself a reasonable length of time, such as a year, to get back into pre-pregnancy shape.
Patience, rehabilitation and sleep are essential when returning to exercise post pregnancy. Listen to your body. Have an exercise plan before you start and remember it is always best to seek professional advice.