Prolapse, much like incontinence, is one of those topics which no-one really likes to talk about. But is so important women understand what’s really going on down there! So we’re going to give you the low down on what it is, how to recognise it, and what to do about it if you have end up with a prolapse…
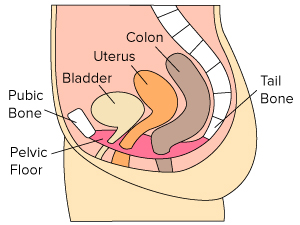
The organs of the pelvis – the bladder, rectum and uterus – are supported within the pelvis by connective tissue (or “fascia”), ligaments and pelvic floor muscles. If these tissues are stretched or torn, and/ or your pelvic floor muscles become weak, your pelvic organs may not be held in place and may bulge down into the vagina. This is called pelvic organ prolapse or POP.
Pelvic organ prolapse is very common. Did you know that up to 50% of women who have given birth will suffer from prolapse? It can also be seen in women who have not given birth and is often associated with straining at stool. Collagen type is also important, and women who are hypermobile (i.e. extra range of motion in a joint or joints) may be predisposed to prolapse.
Women may first notice prolapse when they find a lump or bulge in the vagina and have a sense of dragging or aching. There may be issues with incontinence or difficulty evacuating the bowel. The symptoms are often worse at the end of the day, particularly if you are on your feet all day or doing a lot of bending and lifting. Prolapse often feels better after lying down.
Childbirth is the most common cause of prolapse. When the baby descends through the birth canal, stretching or tearing of the supportive tissue and pelvic floor muscles may take place. However, chronic coughing, a long history of straining at stool/ constipation and heavy lifting, are other factors that can cause prolapse.
Prolapse is named after the organ that has lost its support and is protruding into the vagina. You may hear terms such as urethrocele (when the urethra protrudes into the vagina), cystocele (bladder), rectocele (rectum), enterocele (small intestine), or uterine (uterus) prolapse. However, new terminology makes it easier to understand with terms such as anterior wall (bladder) and posterior wall (rectum) prolapse.
Women are often devastated to learn that they have a prolapse and are sometimes angry that they were not informed about this as a consequence of childbirth. Many have little or no knowledge of prolapse, so education is the key to helping women understand their body and how best to manage it.
Conservative measures such as pelvic floor muscle strengthening, bracing and correct position for defaecation, can help to reduce symptoms of prolapse. Local oestrogen can help with tissue quality in the vagina for women who are breastfeeding or post menopausal. Pessaries, which are a plastic or rubber device inserted into the vagina, can help reduce symptoms of prolapse by supporting the wall of the vagina. Lifestyle changes such as ensuring adequate fluid intake, a well-balanced diet, maintaining a healthy body weight, and avoiding excessive straining, can all help prevent and assist in the management of prolapse. Being aware of safe lifting techniques, bracing before lifting, and avoiding exercises or activities which cause an increase in intra-abdominal pressure are all important as well.
Lastly, surgery may be recommended if the prolapse is significant and not responding to conservative management. In this case referral, to a gynaecologist or urogynaecologist may be necessary – you should speak to your GP about arranging a referral.
We strongly recommended you see a pelvic floor physio if you are experiencing any symptoms of prolapse, as there is a lot that can be done to help reduce and prevent worsening of symptoms. And education is key to understanding any symptoms and being able to take timely and appropriate action.